Women, Hispanic patients at risk for post-surgery emergency visits
Those with health problems also see higher hypoparathyroidism risk
Written by |
Women, Hispanic patients, people who have other health problems, and those who have more lymph nodes removed are at higher risk of emergency visits for hypoparathyroidism after thyroid surgery, a study found.
“Most risk factors identified are not modifiable, but they help identify high-risk patients who could benefit from targeted postoperative care (programs) to reduce unplanned [emergency department] visits,” wrote the researchers, from the University of California, Davis.
The study, “Hypoparathyroidism After Total Thyroidectomy: A Population-Based Analysis of California Databases,” was published in the Journal of Surgical Research.
Some patients develop hypoparathyroidism after thyroidectomy, a surgical procedure to remove all or part of the thyroid gland. This can occur when the parathyroid glands, a group of small glands near the thyroid, are damaged or accidentally removed.
The parathyroid glands produce a hormone that helps control the levels of calcium in the blood. Without enough parathyroid hormone, there is less calcium in circulation, leading to hypoparathyroidism symptoms like muscle cramps and spasms, tingling, and fatigue.
Examining patient records
While hypoparathyroidism is often managed without a hospital stay, some patients require medical care at the emergency department. To understand the factors that lead patients to visit the emergency department, the researchers looked at the medical records of patients who had total thyroidectomy for thyroid cancer.
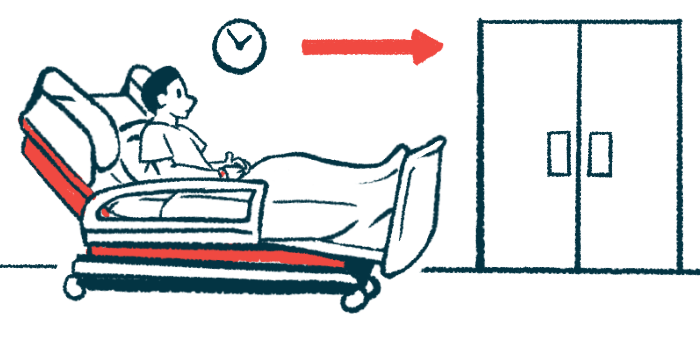
Of 41,502 patients, 588 (1.4%) visited an emergency department due to hypoparathyroidism a median of four days after thyroidectomy. More than two-thirds (67.4%) of a total of 723 visits occurred within one month after surgery, 109 (15.1%) occurred between one and six months, and 127 (17.6%) occurred between six months and two years.
Visits to the emergency department were more common among women and among patients who were Hispanic, younger (aged 18-40), had other health problems, lived in low-income neighborhoods, or had more than four lymph nodes removed, the study found. Living in a higher-income neighborhood was associated with a lower likelihood of needing an emergency department visit.
Being treated at a center not accredited by the American College of Surgeons Committee on Cancer was also linked to more visits to the emergency department.
“[Emergency department] visits for hypoparathyroidism after total thyroidectomy are uncommon, but usually occur shortly after surgery,” the researchers wrote. Certain groups of patients “may benefit from early, targeted interventions,” they concluded.