Hypoparathyroidism tied to cancer-related thyroidectomy mortality
Condition often caused by damaging parathyroid glands during thyroid removal
Slightly less than 20% of people who had their thyroid gland removed had hypoparathyroidism a year after the surgery, according to a 20-year study in Denmark.
An increase in mortality risk was only found when the the surgery was due to cancer, but mortality was unaffected in benign cases. The study, “Hypoparathyroidism and mortality after total thyroidectomy: A nationwide matched cohort study,” was published in Clinical Endocrinology.
A feature of hypoparathyroidism is low parathyroid hormone (PTH) levels. PTH is a key regulator of blood calcium and phosphorus. Low PTH levels lead to low calcium and high phosphorus, resulting in a wide range of symptoms.
The disease is often caused by accidentally damaging the parathyroid glands, four small glands in the neck that produce PTH, during surgery to remove the thyroid gland, a procedure called a total thyroidectomy. Hypoparathyroidism may be transient, or temporary, but can become chronic in some patients.
The condition has been associated with a higher risk of some disorders, including kidney complications, which have been attributed to long-term supplementation with calcium and vitamin D.
Here, researchers in Denmark used population-based registries to study patients who had their thyroid removed between 1998 and 2017 to see if “increased mortality could be attributed to the previously observed higher risk of kidney impairment in [hypoparathyroidism].” A total of 7,883 patients were included, as were 78,830 randomly selected people matched for sex and birth year who served as controls. Hypoparathyroidism, defined as continuous treatment with active vitamin D up to 12 months after surgery, was present in 1,310 patients (16.6%).
Mortality higher in hypoparathyroidism
Most were women (78.6%), had a median age of 52.1, and were followed for a median of 7.1 years. Most thyroid removal surgeries were done in a single procedure (78.2%). Hypoparathyroidism was most commonly observed in these patients, compared with those who’d undergone two or more procedures.
The main causes for removing the thyroid were goiter (44%), the excessive growth of the thyroid gland, cancer (28.9%), and high levels of circulating thyroid hormones (25.9%).
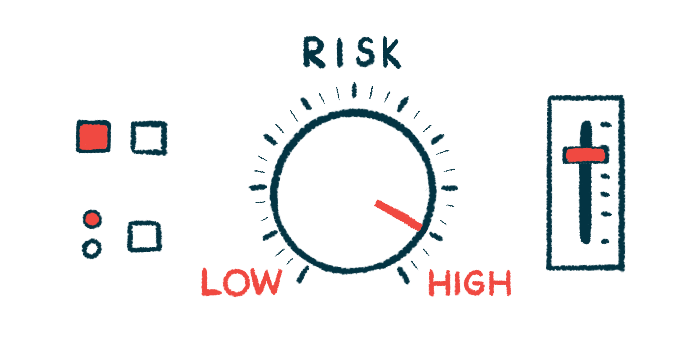
The incidence of all-cause mortality a year after a total thyroidectomy was higher for those with hypoparathyroidism than those without the condition (2.5% vs. 1.6%) or the control group (1.3%). The patients who had surgery still had a higher risk of mortality 10 years later.
After adjusting for potential confounding factors, the risk of death due to any causes after a thyroidectomy was increased by 34% in those who developed hypoparathyroidism. Potential confounders were related to the surgery, hypoparathyroidism and death. They included age, sex, and disorders like diabetes, high blood pressure, obesity, as well as cardiovascular, pulmonary, and autoimmune diseases.
When classifying patients based on the Charlson comorbidity index, only those with hypoparathyroidism, but without coexistent conditions had an increased risk of death, by 35%, compared to matched controls. In patients with multiple comorbidities, mortality risk was either similar or reduced compared with the matched control group.
When considering the cause of surgery, however, mortality risk was 2.48 times higher in thyroid cancer patients. No such effect was seen when surgery was due to benign indications.
“This finding may reflect a well‐known risk of long‐term mortality after thyroid cancer operations,” wrote the researchers who said it was difficult to generalize the study’s conclusions to more ethnically diverse populations because the Danish population is mainly Caucasian.