Long‐term Use of Specific Hormone in Hypoparathyroidism Benefits Bone Remodeling, Study Finds
Long-term treatment with the human recombinant parathyroid hormone (rhPTH) in patients with hypoparathyrodism causes significant and sustained changes in bone remodeling and structural changes to the bone, according to researchers.
Their study, “The Effects of Long-term Administration of rhPTH(1-84) in Hypoparathyroidism by Bone Histomorphometry,” was published in the Journal of Bone and Mineral Research.
Hypoparathyroidism is a rare disease characterized by hypocalcemia (low levels of calcium) and insufficient levels of the parathyroid hormone (PTH).
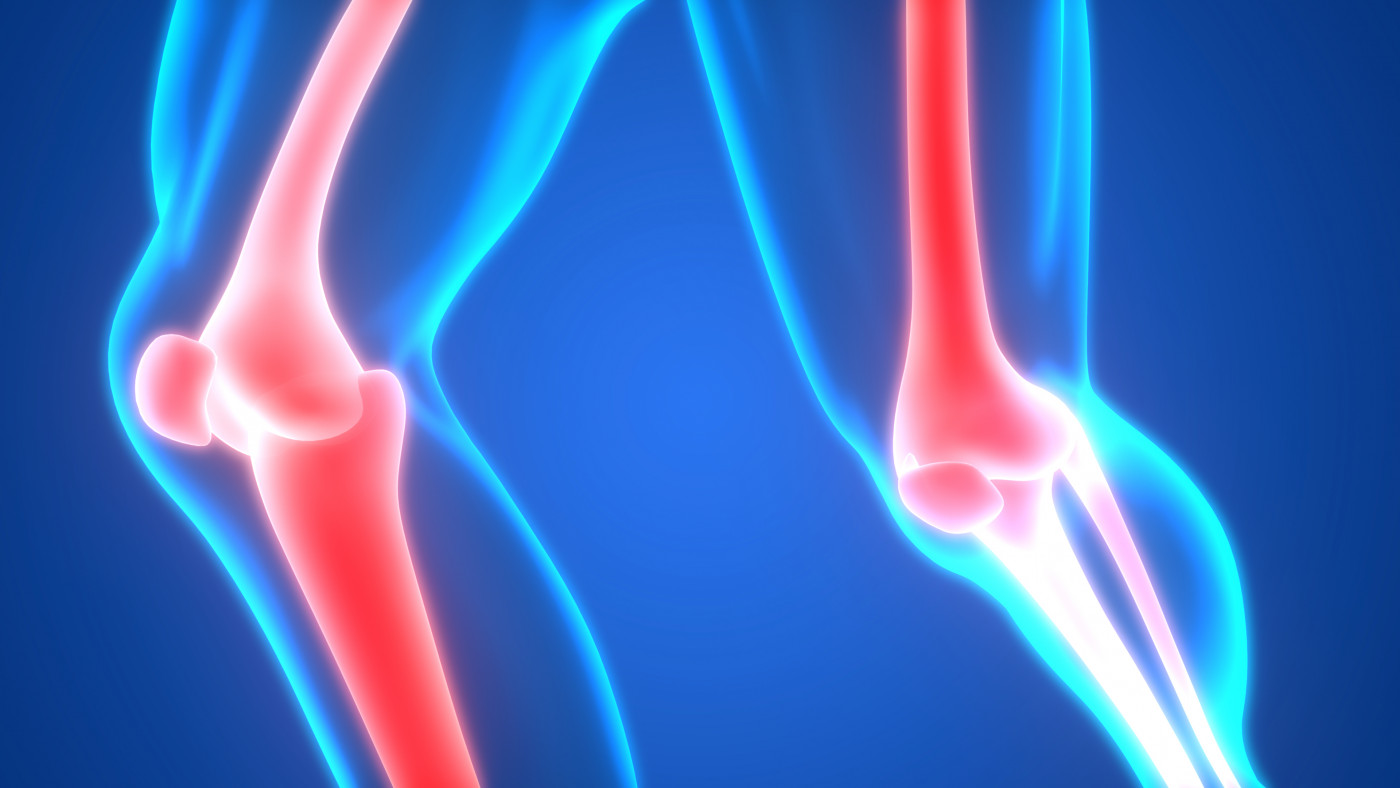
People with hypoparathyroidism exhibit a significant reduction in bone remodeling, a lifelong process in which mature bone tissue is removed from the skeleton — a process called bone resorption — and new bone tissue is formed.
Studies have shown that specific indexes of bone remodeling, such as mineralizing surface and bone formation rate, are significantly suppressed in patients with hypoparathyroidism.
FDA-approved human recombinant PTH (rhPTH, marketed by Shire under the brand name Natpara) — a treatment for hypoparathyroidism — has been shown to significantly improve bone properties after short-term use. Remodeling parameters can improve as early as three months after treatment, and last for at least two years.
However, given the chronic nature of hypoparathyroidism and the likelihood that this hormone will be used long-term, it is important to determine its long-term skeletal effects.
Researchers evaluated changes in bone structure and bone remodeling parameters using bone biopsies from 13 hypoparathyroid patients before and after an average of 8.3 years on rhPTH treatment.
As expected, before they started taking rhPTH, all bone remodeling indexes were significantly suppressed. But after long-term treatment, bone remodeling parameters increased.
Specifically, mineralizing surface increased by 26-fold, and bone formation rate increased by 15-fold. The width of the osteoid (the unmineralized organic component of bone) doubled, and its surface tripled.
Bone resorption — the process by which cells in the bone break down tissue and release minerals — was measured through the extent of eroded surface. Bone erosion increased after treatment, indicating an improvement in bone remodeling.
Treatment also led to significant structural changes, including an increase in cancellous bone volume, a porous bone found at the ends of long bones like the femur.
Some bone remodeling parameters improved so efficiently after rhPTH treatment that they exceeded the values of healthy controls.
These parameters included mineralizing surface, osteoid surface, eroded surface, cancellous bone volume, and trabecular number — small tissue elements that form certain parts of the bone.
“This study has shown, for the first time in a cohort of patients with hypoparathyroidism, that long-term treatment with rhPTH(1-84) induces significant and sustained changes in remodeling and structural indices of bone,” the researchers wrote.
“These data, the first to reflect such long exposure of any PTH for any disease, illustrate that PTH establishes and maintains a new skeletal state for at least 8 years in hypoparathyroidism,” they added.
In the study’s disclosure, three of the nine researchers said they either were consultants for Shire, were on the Shire speakers bureau, or received research support from the company.