Using real-time tech may help ID parathyroid glands during surgery
Trial confirms benefits of using new tool in treating hypoparathyroidism
Written by |
Technology used in real time may help surgeons identify a greater number of parathyroid glands during surgery — including in patients undergoing thyroidectomy, a procedure to remove part or all of the thyroid gland that is a common cause of hypoparathyroidism.
That’s according to a new study that detailed the tech’s use in a clinical trial conducted at four U.S. medical centers.
The technology, called fiber-based near-infrared autofluorescence, or NIRAF, delivers near-infrared light to tissues. It can be used in identifying parathyroid glands, the researchers noted, because these organs emit a stronger autofluorescence signal than other tissues in the neck.
“It is gratifying to now have this large, multicenter clinical trial provide further evidence of [NIRAF technology’s] impact in successfully and efficiently identifying [parathyroid glands] during surgery,” Anita Mahadevan-Jansen, PhD, study author and professor at Vanderbilt University Medical Center in Tennessee, said in a university news story. “It is our ultimate goal to improve the accuracy of endocrine neck surgeries, which will lead to improved patient outcomes.”
The researchers noted that the use of NIRAF “did not significantly impact short-term patient outcomes.” However, the team said “it may be a valuable intraoperative tool for surgeons when other methods for [parathyroid gland] tissue confirmation are unavailable.”
The study, “Detection During Endocrine Neck Surgery A Randomized Clinical Trial,” was published in the journal JAMA Surgery.
Hypoparathyroidism is characterized by reduced levels of the parathyroid hormone (PTH) that helps regulate levels of calcium and phosphorus. PTH is produced by the parathyroid glands, which are small organs located in the neck near the thyroid.
In most cases, hypoparathyroidism is caused by damage to or removal of the parathyroid glands during neck surgery. Long-term complications of the disease include impaired kidney function and irregular heartbeat.
Given these potential complications, it is crucial for surgeons to accurately identify and preserve parathyroid glands during such procedures to reduce the risk of hypoparathyroidism.
Tech, dubbed NIRAF, tested in over 750 surgeries in US trial
Here, a team led by researchers at Vanderbilt conducted a clinical trial assessing the use of NIRAF to identify parathyroid glands during surgery. Specifically, the researchers used the PTeye device, approved by the U.S. Food and Drug Administration in 2018 to assist in the detection of the parathyroid glands.
Carmen Solórzano, MD, the study’s senior author and chair of the department of surgery and director of Vanderbilt Endocrine Surgery, noted that parathyroid glands “can have unpredictable locations and can be found anywhere in the neck from just below the jaw to the chest, near the heart.”
Normal [parathyroid glands] are about the size of a lentil and look like other tissues in the neck, so they can be difficult to locate and identify, even for skilled surgeons.
As such, “relying on eyesight alone during thyroid or parathyroid procedures might not bring the best outcomes,” Solórzano said, adding that “normal [parathyroid glands] are about the size of a lentil and look like other tissues in the neck, so they can be difficult to locate and identify, even for skilled surgeons.”
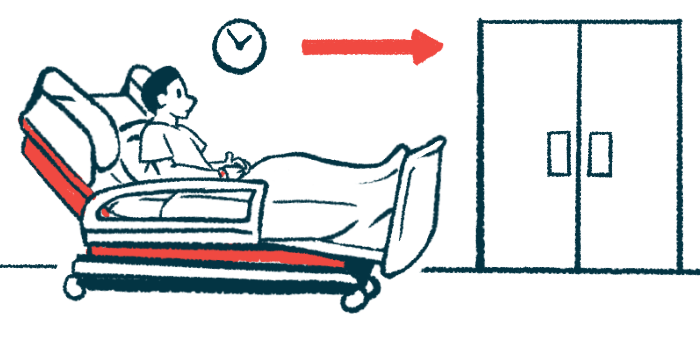
The trial (NCT05579782, NCT05022667, NCT05022641, NCT04281875, NCT04299425, and NCT05152927) was conducted at medical centers in California, Michigan, Tennessee, and Wisconsin. It involved a total of 752 adults, of whom 354 underwent thyroidectomy and 398 had parathyroidectomy — a surgery to remove one or more parathyroid glands, usually due to the production of excessive PTH levels.
The patients having thyroidectomy had a median age of 52, and 75% were women. Those undergoing parathyroidectomy overall were somewhat older, with a median age of 64. Among them, 76% were women.
Number of parathyroid glands ID’d in surgery was higher with NIRAF
In both groups, patients were randomly assigned to surgery using NIRAF or standard surgical care (control group). During thyroidectomies, the average number of parathyroid glands identified per patient was significantly higher in the NIRAF group (3.3 vs. 2.8) than in controls, the researchers found.
Similar results (3.5 vs. 3.2) were seen during bilateral neck exploration, an approach used in cases of overactive parathyroid glands. In both types of surgery, there was an increase in the number of parathyroid glands identified after the use of NIRAF, compared with before the procedure (thyroidectomy: 3.3 vs. 2.7; bilateral parathyroid surgery: 3.5 vs. 3.1)
In contrast, no differences were seen between the groups in duration of surgery and in the number of new cases of hypoparathyroidism, either temporary or at the last follow-up. Also, the rate of accidental removal of parathyroid glands during thyroidectomy was not significantly different when comparing the two groups.
However, during thyroidectomy, the use of NIRAF reduced the need for tissue analysis to confirm the identification of parathyroid tissue, the team noted.
Overall, “the study suggests that … fiber-based NIRAF may help surgeons identify more [parathyroid glands] with high confidence,” the researchers concluded.