Hypoparathyroidism with Pain Mistaken for Type of Arthritis, Case Report Finds
Written by |
A 52-year-old woman with spine and hip pain related to hypoparathyroidism was wrongly diagnosed with spondyloarthritis (SpA) — a type of arthritis that affects the spine — leading to years of unnecessary anti-inflammatory use, a case study reported.
Its investigators said that hypoparathyroidism should be considered when spondyloarthritis is suspected.
The study, “A rare case of spondyloarthropathy: Iatrogenic hypoparathyroidism,” was published in the Turkish Journal of Physical Medicine and Rehabilitation.
Hypoparathyroidism is characterized by low levels of parathyroid hormone, or PTH, produced by the parathyroid glands, four small nodes in the neck behind the thyroid glands. PTH controls calcium levels in the body by modulating the breakdown of bone to release calcium, and regulating how much calcium is absorbed from the diet.
The disorder can be caused by the parathyroid glands being damaged or removed, or it can have genetic origins or be induced by wrongful immune system attacks on the parathyroid glands or PTH.
Typical symptoms include tingling in the fingers and toes, and involuntary muscle spasms and contractions.
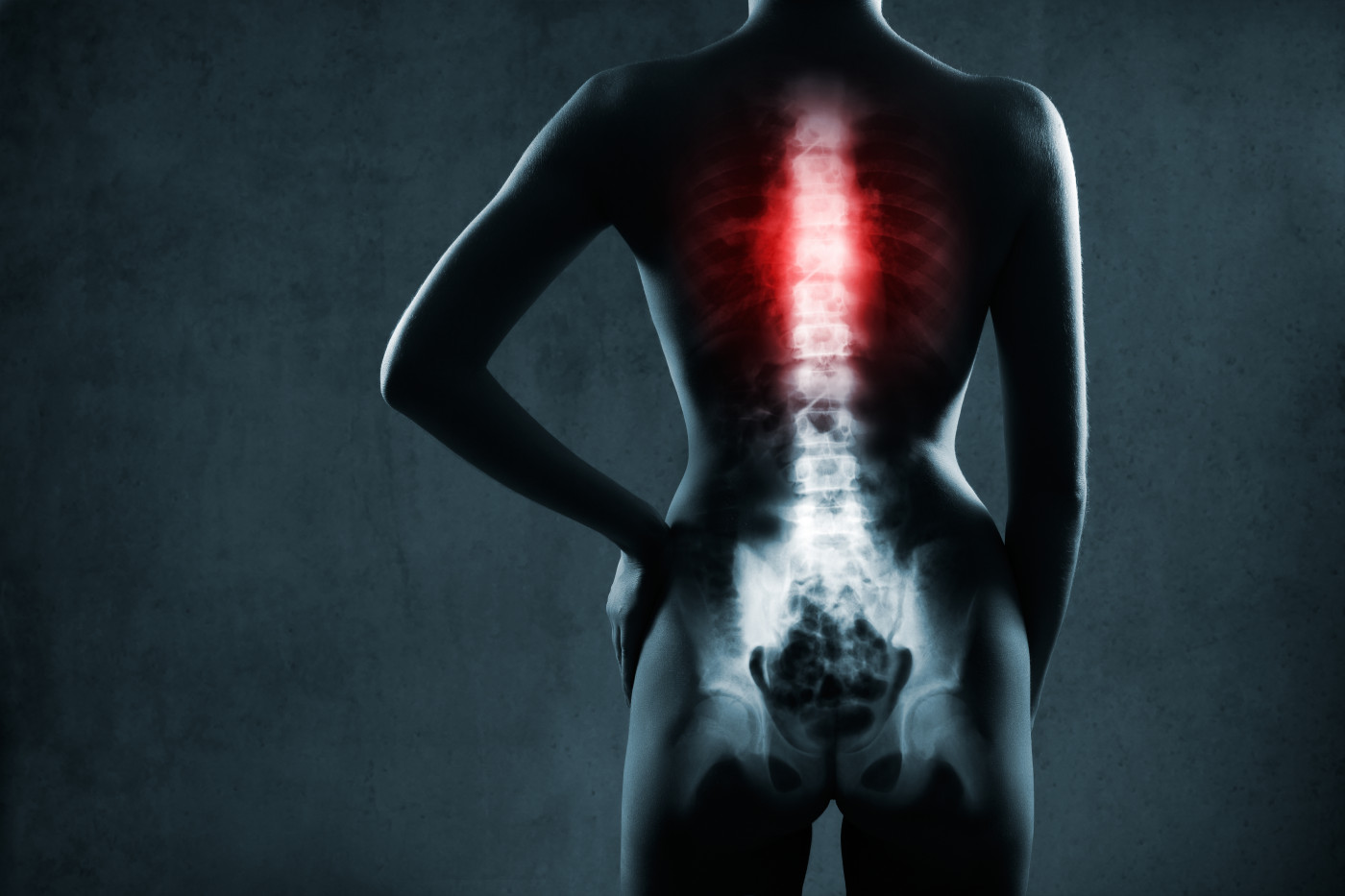
In some cases, patients report widespread pain and problems with posture. X-rays can show a buildup of calcium under the skin, and around joints and muscles of the spine.
These symptoms are also found in people with SpA, an inflammatory condition that mostly attacks the spine. As such, people with these hypoparathyroidism can be misdiagnosed with SpA and unnecessarily treated.
A woman was admitted to research team’s physical medicine and rehabilitation clinic in Turkey. She reported morning stiffness lasting for an hour, as well as pain in the lower back and hips for the past five years.
She was fatigued all day, and experienced muscle cramps and numbness. An initial examination did not find symptoms such as diarrhea, constipation, abdominal pain, fever, night sweating, or weight loss. Her medical history showed she had undergone thyroid and cataract surgery.
The patient had been diagnosed with SpA, which she was treating with nonsteroidal anti-inflammatory drugs (NSAIDs), a common class of pain relievers that include aspirin and ibuprofen.
A physical examination revealed a limited range of motion throughout her spine and hips, and she had tenderness in her feet.
MRI scans found swelling in hip joints. Additional scans found inflammation in her feet, and mineral deposits in the area of the brain known as basal ganglia — which controls processes such as movement, learning, cognition, and emotion.
While her blood cell counts, and liver and kidney function were normal, her calcium, PTH and vitamin D levels in the blood were below normal. Her phosphorus levels were also higher than normal, an additional symptom of hypoparathyroidism.
As a result, the woman was diagnosed with hypoparathyroidism, most likely caused by the thyroid surgery, and was prescribed stretching and strengthening exercises. After being referred to the endocrine and metabolic disease clinic, she was given calcium supplements in the form of calcium carbonate (2 g/day), and an active form of vitamin D called calcitriol (1 microgram/day).
“In conclusion, a diagnosis of hypoparathyroidism-associated SpA is usually delayed in patients being treated with an inflammatory SpA diagnosis,” the investigators wrote. “These treatments do not improve the condition of the patients and can even worsen their symptoms.”
For this reason, “in cases of suspected SpA, levels of calcium, phosphorus and PTH should be investigated,” they added. “Furthermore, the diagnosis should be reconsidered in patients who do not respond to anti-inflammatory and immunosuppressive treatment.”




