ATA Criteria Useful for Grouping Patients by Hypocalcemia Symptoms
Written by |

The American Thyroid Association (ATA) diagnostic criteria for postoperative hypoparathyroidism are useful to doctors in grouping patients based on symptoms, which could help in managing the disease, a study reported.
“However,” the researchers wrote, differentiating patients in this way “may underestimate the actual incidence,” or the number of new cases of postoperative hypoparathyroidism.
The study, “Role of the 2018 American Thyroid Association statement on postoperative hypoparathyroidism: a 5-year retrospective study,” was published in the journal BMC Surgery by a team of researchers in China.
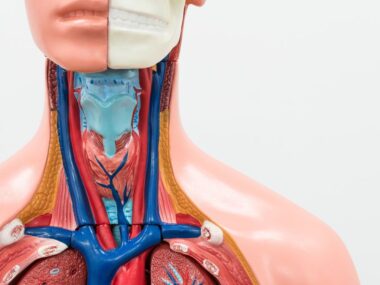
Hypoparathyroidism is characterized by low levels of the parathyroid hormone (PTH) — a hormone secreted by the four parathyroid glands that regulates calcium levels in the body. Its symptoms, which vary widely, are often due to low calcium in the blood (called hypocalcemia).
Thyroidectomy — a surgery to remove part or all of the thyroid gland — is a common cause of hypoparathyroidism. Until recently, however, doctors often used different criteria to diagnose postoperative hypoparathyroidism.
“Many definitions and diagnostic criteria … are found in the existing literature, leading to widespread controversy over its true incidence,” the scientists wrote.
To address this problem, the ATA issued a statement in 2018 regarding the diagnosis, prevention, and treatment of postoperative hypoparathyroidism.
The statement defines three types of postoperative hypoparathyroidism: biochemical hypoparathyroidism (lower-than-normal PTH and calcium levels), clinical hypoparathyroidism (low PTH levels plus symptoms or signs of hypocalcemia), and relative hypoparathyroidism (hypoparathyroidism requiring treatment despite PTH and calcium levels within the normal range).
To find the incidence and risk factors for each type, the researchers looked at the records of patients who underwent a total thyroidectomy due to a papillary thyroid carcinoma — a common thyroid gland tumor — between January 2013 and June 2018 at the same center (West China Hospital of Sichuan University).
Of the 1,749 patients identified, 491 (28.1%) were men and 1,258 (71.9%) were women; their overall age was 41.5. All were followed for at least two years.
Of this group, 521 (29.8%) patients met the ATA diagnostic criteria for postoperative hypoparathyroidism: 458 (26.2%) developed transient hypoparathyroidism or that lasting for less than six months, and 63 (3.6%) had permanent hypoparathyroidism, which lasts beyond six months.
Transient hypoparathyroidism was biochemical in 363 (20.7%) patients, clinical in 72 (4.1%) people, and defined as relative hypoparathyroidism in the other 23 (1.3%).
Permanent hypoparathyroidism was biochemical in eight (0.5%) patients, and clinical in the remaining 55 (3.1%); no one with a permanent condition had relative hypoparathyroidism.
Independent risk factors for transient biochemical hypoparathyroidism were female sex, older age (55 or older), accidental removal of the parathyroid glands, and autotransplantion of two or more parathyroid glands (transplanting two or more glands elsewhere in a patient’s body). Notably, autotransplantation of two or more parathyroid glands was associated with permanent biochemical hypoparathyroidism.
Being age 55 or older, undergoing bilateral central neck dissection, and having a tumor in the isthmus (which connects the two lobes of the thyroid) were independent risk factors for transient clinical hypoparathyroidism.
A reduction of PTH levels of more than 51.1% at one day after surgery increased the risk for relative hypoparathyroidism by almost five times.
No independent risk factor for permanent hypoparathyroidism was found.
“The ATA diagnostic criteria for postoperative hypoPT [hypoparathyroidism] are of great value in differentiating patients by hypocalcemia symptoms and choosing corresponding clinical assistance,” the researchers concluded.