New 5-tier system aims to better guide hypoparathyroidism treatment
Scientists create classification after review of over 12,000 thyroidectomy cases
Written by |
After reviewing more than 12,000 cases of people who underwent surgery to remove all or part of the thyroid gland — a procedure called thyroidectomy, which is known to cause hypoparathyroidism, or low levels of a key hormone — a team of researchers in China has created a classification system to help clinicians provide better, more targeted follow-up treatment for patients.
The researchers found that, while patients undergoing a thyroidectomy may or may not recover from hypoparathyroidism, there are recognizable recovery patterns that can be used to guide timely treatment and prevent or ease symptoms.
To that end, the scientists set forth a five-tiered assessment that doctors can use to identify patients based on risk, and which provides guidelines for how to best manage their cases.
“This large-scale study establishes a precise classification system for postoperative parathyroid function, which may provide a valuable framework to guide clinical management and optimize patient outcomes,” the researchers wrote.
The system was outlined in “The dynamic changes and precise classification of parathyroid function within one year after thyroid cancer surgery,” a study published in the International Journal of Surgery.
Symptoms of hypoparathyroidism result from low levels of parathyroid hormone (PTH), which normally keeps calcium and phosphorus in balance. The condition most commonly occurs after the parathyroid glands are accidentally damaged during thyroidectomy. It’s often temporary, with PTH returning to normal levels.
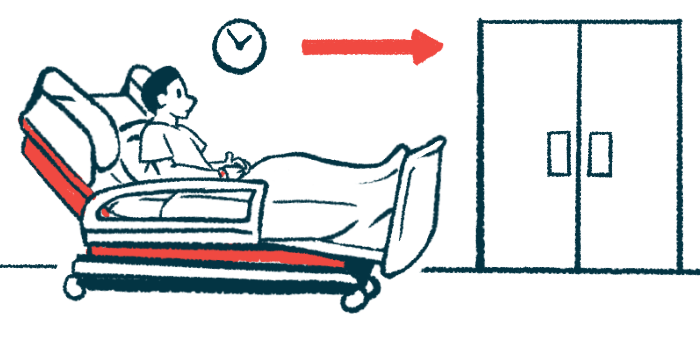
However, the timing of how PTH changes after thyroidectomy is still not well understood, leaving clinicians with little information on how best to manage symptoms — and not knowing which patients might require long-term management.
Scientist ID 5 recovery patterns following thyroidectomy
To better understand recovery patterns, a research team from institutions in China looked at levels of PTH in 12,664 people who had surgery for thyroid cancer at three medical centers in the country between 2012 and 2022.
Slightly more than 8,000 — nearly two-thirds of the patients — had surgery to remove half of the thyroid gland, while the remaining had total thyroidectomy (28%) or subtotal thyroidectomy, which removes most of the thyroid gland (8%). A total of 38,949 measurements for PTH were recorded in the year after surgery.
The data showed that PTH dropped quickly in the first week after surgery, reaching a low point of about 9.7 picograms (pg)/mL. It then increased gradually until the end of the first month. After that, it settled into a slower, more stable pattern, with final levels around 25-29.2 pg/mL — still below those before surgery, the team noted.
“Thus, PTH levels did not fully recover to baseline [initial levels] within the first postoperative year,” the researchers wrote. This suggests that some degree of lasting damage to the parathyroid glands is common, according to the team.
Based on the lowest point reached for PTH after surgery and the new baseline PTH — the stable levels reached sometime after the first month — the researchers identified five different trends of recovery patterns, divided into three types.
- Type I represented preserved parathyroid function, while Type II marked mild damage with parathyroid function within normal limits.
- Type IIIA and IIIB represented different levels of hypoparathyroidism, meaning the glands did not produce enough PTH, but with varying degrees of recovery.
- Type IIIC represented persistent, severe hypoparathyroidism that did not ease over time.
According to the team, more extensive surgery, removal of lymph nodes, moving parathyroid tissue to another location during surgery (called autotransplantation), and low levels of PTH before surgery increased the risk of poor recovery. These factors were combined into a prediction tool called a nomogram.
‘Tailored clinical management strategies’ vary by type
For the researchers, the recommended care plan is straightforward. Under their plan:
- Type I needs no follow-up.
- Type II should be monitored during the first month and treated only if symptoms appear.
- Type III requires calcium and close monitoring during the first month, with subsequent management depending on recovery type.
- Type IIIA usually recovers within one month.
- Type IIIB, marked by partial recovery within the first month, may stop supplements once PTH levels normalize.
- Type IIIC needs long-term calcium and monitoring.
“We established a five-type classification system of postoperative PTH trajectories, developed a predictive model to identify patients at risk, and proposed tailored clinical management strategies,” the researchers wrote, noting that it built on the study’s earlier findings and was based on the largest patient population to date.
“This classification, together with the predictive model developed, provides a framework for tailored postoperative monitoring and intervention. By enabling more precise risk stratification, it offers a means to optimize clinical decision-making,” the team concluded.





