PGA Procedure Tied to Higher Risk of Immediate Hypoparathyroidism
bangkoker/shutterstock
A routine procedure called PGA — for parathyroid gland autotransplantation — often done following surgery to remove the thyroid gland, is associated with a higher risk of immediate hypoparathyroidism, a study shows.
However, PGA did not raise the risk of permanent hypoparathyroidism, or that lasting more than six months. And, in turn, this risk was significantly increased with no use of carbon nanoparticles — commonly used to help surgeons more easily locate the parathyroid glands so as not to remove them — and unintentional parathyroid removal.
According to researchers, these findings support the PGA procedure as a way to preserve parathyroid function and avoid permanent hypoparathyroidism following thyroid removal.
The findings also emphasize the importance of identifying the parathyroid glands during surgery to avoid inadvertent damage.
The study, “The Effect of Parathyroid Gland Autotransplantation on Hypoparathyroidism After Thyroid Surgery for Papillary Thyroid Carcinoma,” was published in the journal Cancer Management and Research.
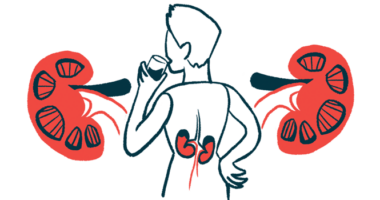
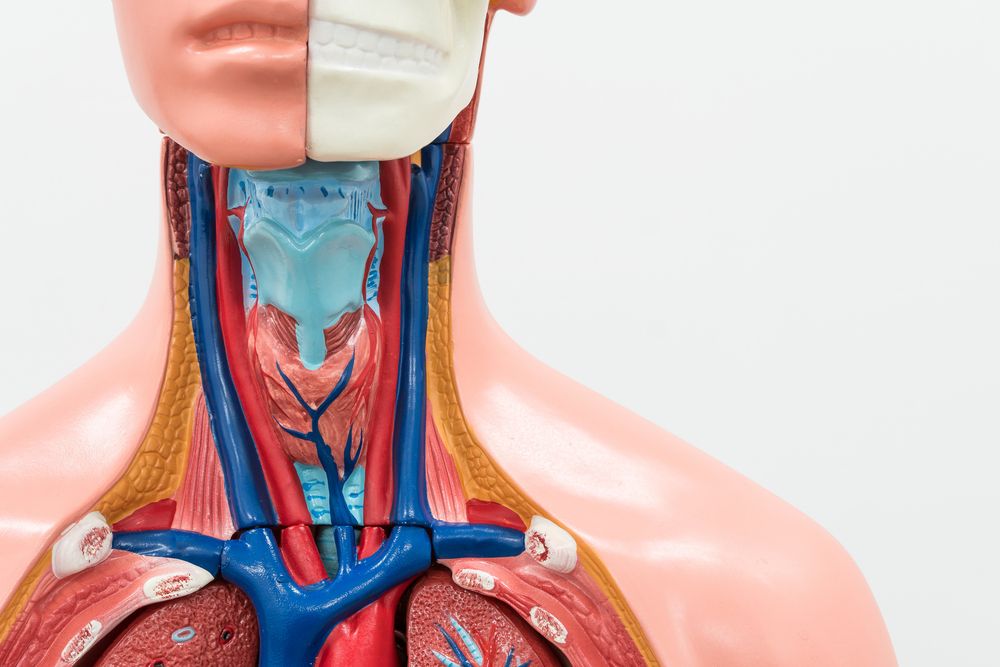
Thyroidectomy, or the surgical removal of all or part of the thyroid gland, can lead to the unintentional removal of the neighboring parathyroid glands (two at each side of the neck) and to chronic hypoparathyroidism, or low levels of the parathyroid hormone (PTH).
Given that PTH regulates calcium levels in the body, low or no levels of PTH may cause post-surgery calcium deficiency.
Preserving the parathyroid glands has remained an important strategy for maintaining normal PTH and calcium levels after surgery. When these glands are damaged or unintentionally removed during surgery, they can be transplanted into the muscle of the neck or forearm in an attempt to normalize PTH production.
This routine procedure, called parathyroid gland autotransplantation or PGA, has been reported to effectively reduce the occurrence of permanent hypoparathyroidism. But some studies found no such benefits or even an opposite effect.
To address this discrepancy, and learn more about PGA’s effects, a team of researchers in China retrospectively analyzed data from 658 people who underwent a total thyroidectomy due to a thyroid tumor (cancer). The patients had surgery between January 2014 and December 2018 and were followed for at least six months afterward.
The patients’ demographic characteristics, pre- and post-surgery clinical and blood work information, and surgery details were analyzed. Specifically, the team examined the number of transplanted parathyroid glands and the number of parathyroids inadvertently removed and lost.
The investigators then assessed the effects of PGA and the number of transplanted parathyroids in post-operative hypoparathyroidism, as well as potential risk factors.
Among the patients, 468 were female and 190 were male; their mean age was about 40. When PGA was performed, pieces of parathyroids were introduced into the patients’ neck muscles.
The results showed that 216 patients did not undergo PGA. In all, 587 parathyroid glands were autotransplanted among 442 patients, and 83 parathyroids were unintentionally removed and lost among 80 patients. A total of 314 underwent a transplant of one parathyroid gland, 111 of two glands, and 17 patients of three glands.
Patients undergoing PGA were significantly more likely to show immediate hypoparathyroidism following surgery than those not undergoing the procedure.
Notably, the more parathyroid glands that were transplanted, the significantly higher was the occurrence of immediate hypoparathyroidism. Additionally, the more glands transplanted, the longer was the hospital stay.
Specifically, immediate hypoparathyroidism was reported in nearly one-third of patients not undergoing PGA, versus 52.9% among those who had one parathyroid gland transplanted, 65.8% in those who had two glands transplanted, and 82.4% among patients who had three of their glands transplanted.
However, the rate of permanent hypoparathyroidism was similar between patients who did not undergo PGA (1.4%) and those who underwent the procedure (0–1.3%), highlighting that PGA did not affect the frequency of permanent hypoparathyroidism, regardless of the number of parathyroids transplanted.
Notably, previous studies showed that it took at least one month for the transplanted parathyroid glands to recover their function.
These new findings suggest that, overall, working parathyroid gland tissue in the body during this period is increasingly reduced with more parathyroids being transplanted, but this does not affect the full recovery of PTH production later on.
The researchers hypothesized that their findings also might be associated with the fact that most patients undergoing PGA had at least three working parathyroid glands after surgery, regardless of whether they were preserved in site or autotransplanted.
Also, among patients who did not undergo PGA, the fewer parathyroid glands unintentionally removed and lost, the lower was the risk of post-operative immediate hypoparathyroidism.
There were no significant differences in the occurrence of immediate and permanent hypoparathyroidism between patients with and without one preserved parathyroid on site after undergoing PGA.
Besides PGA, female sex and inadvertently removing parathyroids were found to be independent risk factors for post-surgery immediate hypoparathyroidism. Unintentional parathyroid removal, as well as non-use of carbon nanoparticles, significantly increased the risk of permanent hypoparathyroidism.
Overall, these findings highlight that PGA significantly increases the risk of post-operative immediate hypoparathyroidism, “and the more parathyroid glands are transplanted, the more likely the immediate hypoparathyroidism occurs,” the researchers wrote.
However, PGA “does not affect permanent hypoparathyroidism when three or more functional parathyroid glands are reserved regardless of whether they are preserved in site or autotransplanted,” they added.
“The use of carbon nanoparticles could help to reduce the incidence of permanent hypoparathyroidism and the parathyroid gland should be identified as much as possible to avoid being inadvertently resected,” the researchers concluded.