Low PTH Levels Right After Thyroidectomy Linked to Permanent Hypoparathyroidism, Study Suggests
Noting low parathyroid hormone (PTH) levels on the first day after total thyroidectomy can be useful for identifying patients at risk of developing permanent hypoparathyroidism, a single-center study in Italy has found.
The findings were described in the report “Correlation between iPTH levels on the first postoperative day after total thyroidectomy and permanent hypoparathyroidism: our experience,” and published in the journal Open Medicine.
Hypoparathyroidism is a common complication following total thyroid gland removal, or thyroidectomy. It is characterized by reduced levels of the parathyroid hormone (PTH), which results in low blood levels of calcium (hypocalcemia), and higher levels of blood phosphate (hyperphosphatemia).
This can lead to a number of health problems, ranging from mild to severe or even potentially fatal, including numbness on face and hands, convulsions and suffocation. People with prolonged excess calcium also risk developing kidney stones, chronic kidney failure, heart problems, brain calcifications, cataracts, and dental abnormalities.
Most of the time, hypoparathyroidism due to thyroidectomy reverses naturally within a few months. However, in a minority of patients — up to 10% — this complication persists for long periods or even permanently.
To avoid the consequences of chronic blood calcium deficiency, long-term therapy with calcium and vitamin D “are mandatory,” along with a careful follow-up, researchers said. However, long-term calcium therapy also can cause unwanted side effects.
To improve the care management for these patients, “it would be very useful to be able to predict the risk of permanent hypoparathyroidism at an early stage after surgery,” the researchers said.
However, there are no reliable markers, traceable just after surgery, to help identify those at risk.
Attempting to fill this gap, the researchers investigated if blood levels of intact PTH (iPTH) — the biologically active form of PTH that is secreted when calcium levels are low — one day after surgery could be a good predictor of permanent hyperparathyroidism.
The investigators retrospectively analyzed iPTH levels of 75 patients undergoing thyroidectomy in Policlinico Universitario Casula, in Italy, between January 2017 and February 2018. All subsequently developed hypoparathyroidism.
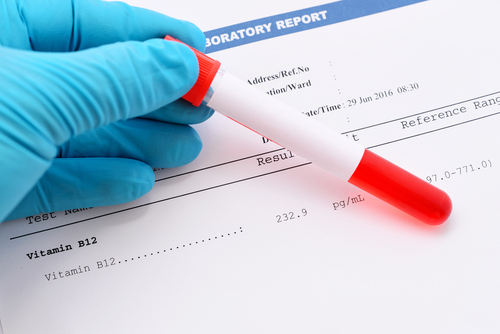
These individuals were divided into two groups, based on their iPTH values on the first day post-surgery. Group A included those with iPTH levels lower than 6.3 pg/mL, or undetectable (64 patients). Those in group B had iPTH concentrations of 6.3 pg/mL or higher (11 patients). The normal range of blood iPTH is 10-65 pg/mL.
Only patients in group A, which had the lowest iPTH levels, developed hypoparathyroidism. In this group, 14 out of 64 individuals developed the complication (21.88%), in contrast with none in group B.
This means that in this group of patients, undetectable iPTH values (lower than 6.3 pg/mL; group A) had a 100% sensitivity for predicting the development of permanent hypoparathyroidism.
Nevertheless, this measure still had a low specificity (18.03%), and a low positive predictive value (21.88%) — which translates as the probability that subjects with a positive test truly will have the complication. Therefore, a low iPTH is not enough to be a “strong predictor of this condition,” the researchers said.
However, given its high sensitivity — all patients who later developed permanent hyperparathyroidism had a low iPTH — this cut-off value (6,3 pg/ml) “can be useful to identify patients at risk of developing this complication … who require a careful follow-up,” the team concluded.