Asymptomatic Hypoparathyroidism in Thalassemia Patients Is Not Uncommon, Researchers Find
Screening for asymptomatic hypoparathyroidism should be considered in transfusion-dependent thalassemia patients to allow for early disease detection and intervention, researchers suggest.
Their study, “Under-recognized Hypoparathyroidism in Thalassemia,” was published in the Journal of Clinical Research in Pediatric Endocrinology.
The occurrence of asymptomatic hypoparathyroidism, defined as low levels of calcium in the blood without elevated parathyroid hormone (PTH) levels, may be more common than once thought in patients with thalassemia, and could be under-recognized by clinicians.
Patients with moderate to severe thalassemia often undergo regular blood transfusions and are said to have transfusion-dependent thalassemia.
These regular blood transfusions result in elevated blood phosphate levels, causing the secretion of the hormone fibroblast growth factor-23 (FGF-23). This in turn reduces phosphate reabsorption by the kidneys.
FGF-23 also reduces PTH secretion by the parathyroid glands.
To characterize asymptomatic hypoparathyroidism, its prevalence and associated biochemical profiles in thalassemia patients, researchers from Mahidol University in Thailand, studied 66 transfusion-dependent thalassemia patients (their median age was 13.5) who had received regular transfusions every three to four weeks, as well as 28 healthy controls (median age 8.9).
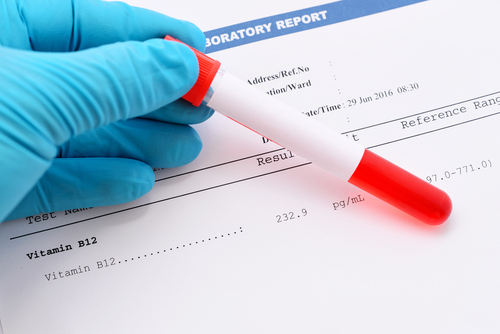
Transfusion-dependent thalassemia patients had significantly lower levels of calcium and FGF-23 than healthy controls, while no significant differences were observed regarding phosphate, PTH, and 25-OHD (used to determine vitamin D levels).
Asymptomatic hypoparathyroidism was found in 25 (38%) out of the 66 thalassemia patients, a significantly higher prevalence than previously reported (0.5% to 7.6%).
There were no significant differences in weight, height, age of onset of transfusion, and body mass index (BMI) between those with asymptomatic hypoparathyroidism and normal parathyroidism.
FGF-23 levels were, however, lower in the hypoparathyroidism group.
Despite the small number of patients and non-age-matched controls used in this study, researchers conclude that “hypoparathyroidism was not uncommon in patients with transfusion-dependent thalassemia.”
As such, “screening for asymptomatic mild hypocalcemia without elevation of parathyroid hormone should be considered in transfusion-dependent thalassemia for early detection and proper treatment,” the authors concluded.